What Is MRSA? Your Complete Guide to Symptoms, Causes & Risks
Are you concerned about a skin infection that won’t heal, or perhaps you’ve been told you need screening before a hospital procedure? The term ‘MRSA’ can sound alarming, and navigating the complex and often worrying information online is a challenge. This uncertainty understandably leads to many questions about MRSA and its potential impact on your health. It’s a term frequently mentioned in clinical settings but not always clearly explained, leaving many people feeling anxious and unsure where to turn for trusted advice.
This comprehensive guide is designed to provide the clarity you need. In the following sections, we will calmly and professionally explain what MRSA is, how to confidently recognise the symptoms of an infection, and why screening is a crucial preventative step. Our goal is to replace medical jargon with straightforward facts, empowering you with the knowledge to feel reassured and in control of your health decisions.
What is MRSA? A Simple Explanation
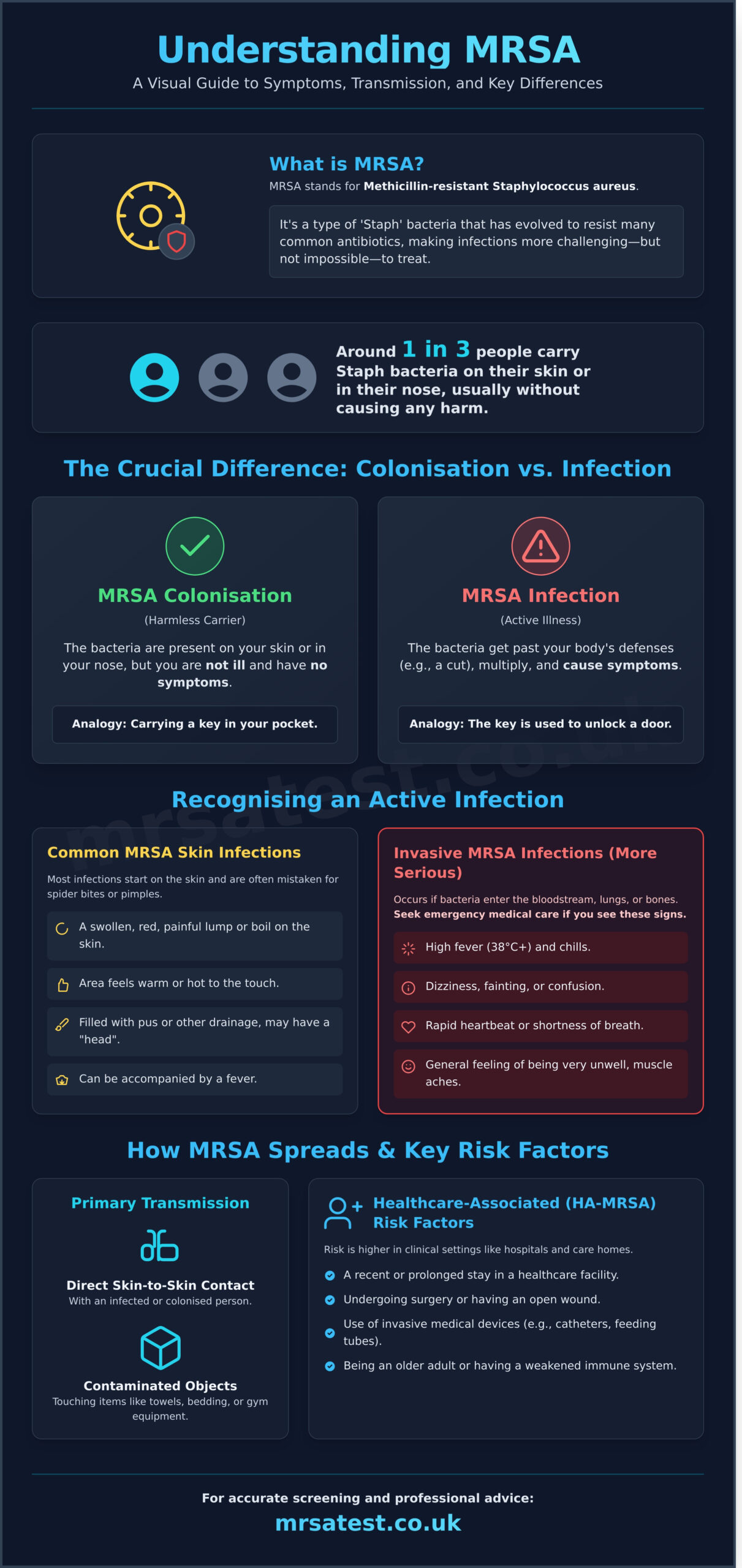
MRSA is a term you may have heard in a healthcare setting, and it’s natural to have questions. In simple terms, MRSA stands for Methicillin-resistant Staphylococcus aureus. It is a specific strain of a common bacterium called Staphylococcus aureus, often referred to as ‘Staph’. What makes MRSA different is its resistance to methicillin and other common antibiotics that are typically used to treat Staph infections.
However, it’s important to know that Staph bacteria themselves are very common. Around one in three people carry Staph on their skin or in their nose, usually without causing any harm. The key is to understand the crucial difference between simply carrying the bacteria (colonisation) and having an active illness (infection).
MRSA Colonisation vs. MRSA Infection
MRSA colonisation means the bacteria are present on or in your body, but you are not ill and have no symptoms. For a healthy person, being colonised with MRSA is typically not a problem and requires no treatment. The bacteria are simply living harmlessly on the skin’s surface or in the nasal passages without causing any issues.
An MRSA infection occurs when the bacteria manage to get past your body’s natural defences-for example, through a cut, wound, or surgical site-and begin to multiply, causing symptoms. Think of it like this: being colonised is like carrying a key in your pocket. An infection is when that key is used to unlock a door and enter a restricted area. Understanding the distinction between MRSA colonisation and an active infection is the first step in managing your health.
Why is Antibiotic Resistance a Concern?
Antibiotic resistance develops when bacteria evolve in response to the use of these medicines. This resistance is what distinguishes MRSA and makes it a notable concern, particularly in hospitals and care homes where people may have weakened immune systems. Because it doesn’t respond to some of the most commonly prescribed antibiotics, an MRSA infection can be more challenging to treat than other bacterial infections.
While this sounds serious, it is important to remain calm. Harder to treat does not mean impossible to treat. There are still several effective antibiotics available that can successfully clear MRSA infections. A doctor will use lab test results to identify the specific strain and prescribe the correct medication to ensure a safe and effective recovery.
Recognising the Symptoms and Signs of an MRSA Infection
It is important to understand the difference between being colonised with MRSA and having an active MRSA infection. An individual who is colonised carries the bacteria on their skin or in their nose but experiences no symptoms and feels perfectly well. An active infection only occurs when the bacteria breach the body’s defences, such as through a cut or wound, and begin to multiply. Recognising the signs of MRSA and seeking timely medical advice are crucial for effective treatment.
The symptoms of an active MRSA infection depend entirely on which part of the body is affected. The infection can range from a minor skin issue to a life-threatening illness. For a detailed exploration of MRSA symptoms and causes, a trusted medical resource like the Mayo Clinic offers comprehensive guidance.
Common MRSA Skin Infections
Most MRSA infections begin on the skin. They often start as small, red bumps that can quickly turn into painful, swollen abscesses or boils. Many people initially mistake these bumps for common spider bites, pimples, or cysts. Key signs of an MRSA skin infection include:
- A swollen, red, and painful lump or bump on the skin.
- The area feels warm or hot to the touch.
- The centre of the bump may be filled with pus or other drainage and have a distinct head.
- The infection can be accompanied by a fever.
These infections are most common in areas with more hair, such as the armpits, groin, and back of the neck, or on skin that has been broken by a cut, scrape, or wound.
Invasive MRSA Infections (More Serious)
A more severe, or invasive, infection can occur if MRSA bacteria enter deeper into the body, such as the bloodstream, lungs, or bones. This is a serious medical situation that requires immediate attention. Systemic symptoms often develop, indicating the infection is spreading. Be alert for signs such as:
- A high fever (38°C or above) and chills
- Dizziness, fainting, or confusion
- A general feeling of being very unwell
- Muscle aches and pains
- Rapid heartbeat or shortness of breath
These symptoms can signal dangerous conditions like a bloodstream infection (sepsis), pneumonia, or a bone infection (osteomyelitis). If you or someone you know exhibits signs of a serious invasive infection, it is vital to seek emergency medical care without delay.
How is MRSA Transmitted? Causes and Key Risk Factors
Understanding how MRSA spreads is the first step toward effective prevention. The bacteria are primarily transmitted through direct skin-to-skin contact with someone who has an MRSA infection or is colonised with the bacteria (carrying it on their skin without symptoms). It can also spread indirectly by touching objects that have been contaminated by an infected person, such as towels, bedding, or gym equipment.
While the bacteria can be present without causing harm, certain factors significantly increase the risk of it leading to an infection. The risks associated with MRSA and how it is acquired are typically categorised into two distinct settings: healthcare environments and the wider community.
Healthcare-Associated MRSA (HA-MRSA)
As the name suggests, HA-MRSA is acquired within clinical environments like hospitals, GP surgeries, and care homes. These settings can pose a higher risk because patients may have weakened immune systems or open wounds from surgery. Pre-operative screening is a crucial safety measure to identify and manage MRSA before a procedure.
Key risk factors for HA-MRSA include:
- A recent or prolonged stay in a hospital or other healthcare facility.
- Undergoing surgery or having an open wound.
- The use of invasive medical devices, such as feeding tubes or urinary catheters.
- Being an older adult or having a compromised immune system.
Community-Associated MRSA (CA-MRSA)
CA-MRSA refers to infections that occur in healthy individuals who have not recently been in a healthcare setting. Transmission often happens in places where people have frequent and close skin contact. Good personal hygiene is the most effective way to minimise risk.
Common risk factors for CA-MRSA include:
- Participating in high-contact sports like rugby or wrestling.
- Living in crowded or close-quarter conditions, such as university halls or military barracks.
- Sharing personal items that touch the skin, including razors, towels, and athletic gear.
- Poor hygiene practices, which allow the bacteria to spread more easily.
How to Know for Sure: MRSA Diagnosis and Screening
A red, swollen, or painful area of skin can cause concern, but it’s important to remember that MRSA cannot be diagnosed by sight alone. Many common skin infections can look similar, and self-diagnosis can lead to unnecessary anxiety or delayed treatment. Definitive confirmation requires a laboratory test to accurately identify the specific strain of staph bacteria. Understanding the diagnostic process for mrsa and the options for screening can provide clarity and peace of mind.
The Clinical Diagnosis Process
To get a diagnosis, a healthcare professional will first collect a sample from the relevant area. This is a straightforward procedure, typically involving a sterile swab wiped across a wound, skin lesion, or inside the nostrils. For suspected internal infections, a blood, urine, or tissue sample might be necessary. This sample is then securely sent to an accredited laboratory for precise analysis using one of two primary methods:
- Culture Test: This is the gold-standard method. The sample is placed on a nutrient-rich plate (a culture) and incubated to encourage any bacteria present to grow. Technicians can then identify MRSA colonies and test their antibiotic resistance. While highly reliable, this process typically takes 48-72 hours.
- PCR (Rapid) Test: A Polymerase Chain Reaction test is a modern molecular technique that looks for the bacteria’s DNA. It is significantly faster, often delivering results within 24 hours, making it ideal when time is critical.
Pre-Operative MRSA Screening at Home
Many UK hospitals and private clinics require patients to be screened for MRSA colonisation before a planned surgery or hospital admission. This is a crucial safety protocol designed to protect you and other patients. Identifying MRSA carriers beforehand allows medical staff to implement measures that significantly reduce the risk of surgical site infections. Preventing the introduction of mrsa and managing its presence is a key part of modern patient safety.
You can now complete this essential screening process conveniently and discreetly without a trip to a clinic. An at-home MRSA test kit allows you to collect your own sample-usually a simple swab of the nostrils and sometimes the groin or armpit-in the privacy of your home. The sample is then posted in pre-paid, confidential packaging to a UKAS-accredited laboratory for analysis, ensuring you receive fast, accurate results. Learn more about our simple and confidential MRSA test kits.
Effective Prevention and Management Strategies
While an MRSA diagnosis can be concerning, it is important to remember that infections are both preventable and treatable. The most effective approach is to minimise the risk of transmission through proactive, simple hygiene practices. By understanding how to protect yourself and others, you can significantly reduce the likelihood of contracting or spreading the bacteria.
For individuals diagnosed with an infection, adhering strictly to medical guidance is the key to a successful recovery. Below, we outline the essential strategies for prevention and provide a brief overview of how MRSA is managed by healthcare professionals.
Key Prevention Techniques
Implementing good hygiene is the cornerstone of MRSA prevention in both community and healthcare settings. These simple habits can make a significant difference:
- Consistent Hand Hygiene: Wash your hands thoroughly with soap and warm water for at least 20 seconds. If soap and water are not available, use an alcohol-based hand sanitiser containing at least 60% alcohol.
- Proper Wound Care: Keep any cuts, grazes, or breaks in the skin clean and covered with a sterile bandage or dressing until they have healed. Avoid touching or picking at wounds.
- Do Not Share Personal Items: Avoid sharing items that come into contact with skin, such as towels, razors, flannels, and athletic equipment.
- Clean Your Environment: If someone in your household has an MRSA infection, regularly clean and disinfect frequently touched surfaces. Wash their bedding, towels, and clothing separately on a hot wash cycle.
An Overview of MRSA Treatment
It is essential to understand that treatment for MRSA must be directed by a qualified healthcare professional, such as your GP. The specific approach depends entirely on the type, location, and severity of the infection. A minor skin boil, for example, may only require professional draining in a clinical setting.
If an antibiotic is necessary, doctors will not use common penicillin-based drugs. Instead, they prescribe specific antibiotics that laboratory tests have shown to be effective against the particular strain of MRSA. For both skin infections involving MRSA and more invasive conditions, it is crucial to complete the entire course of medication as prescribed to ensure the infection is fully cleared. If you have concerns about exposure or require screening before a hospital procedure, you can test for MRSA from the comfort of your own home to get a clear and accurate result.
Proactive MRSA Screening: Your Path to Peace of Mind
Understanding Methicillin-resistant Staphylococcus aureus is the first and most crucial step toward protecting your health. We’ve covered how to recognise the symptoms, the key risk factors for transmission, mrsa and the effective strategies for prevention. This knowledge empowers you to take proactive steps, especially if you or a loved one are preparing for a hospital stay or have been identified as being at higher risk.
For those seeking certainty, early screening provides definitive peace of mind. Our service offers a fast, reliable, and confidential way to test for MRSA from the comfort of your own home. Your kit arrives in discreet packaging with free shipping, and your sample is processed by a trusted, UKAS-accredited UK laboratory, ensuring accurate results you can depend on.
Take control of your health today. Order your confidential at-home MRSA test kit today.
Frequently Asked Questions About MRSA
Can MRSA go away on its own?
Minor MRSA skin infections may occasionally resolve without treatment, particularly in healthy individuals. Similarly, MRSA colonisation, where the bacteria live on the skin without causing illness, can also clear naturally. However, it is crucial not to self-diagnose. If you suspect an MRSA infection, characterised by red, swollen, or painful skin, you must seek professional medical advice from your GP or the NHS. Prompt treatment is key to preventing more serious complications.
Is MRSA curable?
Yes, MRSA infections are treatable and curable. While MRSA is resistant to some common antibiotics, other effective options are available. Treatment for skin infections often involves draining the abscess and a course of specific antibiotics prescribed by a doctor. For MRSA colonisation, a process called decolonisation may be recommended, which uses antiseptic body washes and nasal ointments to eliminate the bacteria. A healthcare professional will determine the most appropriate treatment plan.
Can you have MRSA and not know it?
Yes, it is very common to carry MRSA on your skin or in your nose without having any signs of illness. This is known as MRSA colonisation or being a “carrier.” The bacteria are harmlessly present but can pose a risk if they enter the body through a cut or wound, or if you are preparing for surgery. This is why pre-operative screening is so important in UK hospitals and why confidential at-home testing can provide valuable peace of mind.
How long does MRSA live on surfaces like towels or bedding?
MRSA is a resilient bacterium that can survive on surfaces for hours, days, or even weeks, depending on the conditions. On fabrics like towels, bedding, and clothing, it can remain viable for an extended period, especially in a moist environment. Regular, thorough cleaning is vital for prevention. Washing linens at a high temperature (at least 60°C) and using disinfectants on hard surfaces can effectively kill the bacteria and reduce the risk of transmission within the home.
What is the difference between Staph and MRSA?
Staphylococcus aureus, often shortened to “Staph,” is a common type of bacteria found on the skin of many healthy people. MRSA stands for Methicillin-resistant Staphylococcus aureus. Essentially, MRSA is a specific strain of Staph that has developed resistance to methicillin and other common antibiotics in the same class. This resistance means that standard treatments are ineffective, and doctors must use different, more specific antibiotics to successfully treat an MRSA infection.
Who is most at risk of getting a serious MRSA infection?
Individuals with weakened immune systems are most susceptible to serious MRSA infections. This includes hospital patients, particularly those undergoing surgery, with intravenous drips, or who have open wounds. Residents of care homes, people with chronic conditions like diabetes or kidney disease, and individuals who have frequent skin-to-skin contact in sports are also at a higher risk. A strong immune system is a critical line of defence against the bacteria causing a more invasive infection.